Psoriatic arthritis (PsA) may significantly change a person's life as one might need long-term treatment to control the symptoms. Depending on the intensity of pain and stiffness, it may become difficult or take longer to perform day-to-day work. Living with PsA, even simple changes to the usual routine can help.
EATING WELL AND MAKING THE RIGHT FOOD CHOICES
PsA affects major joints, which may become swollen and painful. If left untreated for an extended period, they can become damaged. For people with inflammatory conditions, eating certain foods may either lower inflammation or cause even more damage. Experts suggest that definite dietary choices can help reduce disease severity in PsA. Here are some suggestions on foods to eat and avoid and several diets to try for the management of PsA.
Here are a few suggested food items to include :
Anti-inflammatory omega-3s
Present in nuts and fatty fishes like salmon.It helps reduce the pain, joint tenderness and redness.
High-antioxidant foods
Colourful fruits and veggies help to reduce swelling.
High-fiber whole grains
Helps to prevent obesity, which is a risk factor for PsA.
Here are a few food items to avoid:
Red meat
Causes weight gain, swelling.
Processed food
Processed food and drinks are high in excess sugar, salt, and fat, which could cause inflammation.
Foods that cause intolerance and allergies
Such foods activate the immune system and can cause generalized swelling in the body. In order to manage the disease better, stay away from foods that may cause an allergic reaction.
LIFESTYLE CHANGES
Self-Care
Intense and long-term joint pain and stiffness can prevent a person from doing daily work like going to the office or school, and caring for their family. Handling these difficulties can be overwhelming and stressful. Depression and anxiety are common among people with psoriasis and PsA. There are multiple approaches and tools available to improve the quality of life and general state of mind despite these conditions. A part from getting the right treatment, taking out time for self-care can make a big difference. Here are some ways in which patients with PsA can take care of themselves:
Be as active as possible
Exercising can have a positive impact on PsA symptoms. With an added benefit of weight loss, one can manage PsA more effectively.
Give the body enough nutrients
One symptom of PsA is fatigue, which may demoralize a person. Healthy eating can help combat PsA-associated fatigue and other physical symptoms like pain and swelling. Furthermore, it is advisable to limit alcohol intake and quit smoking as it can interfere with the medications or increase side effects. It may also result in a flare-up of the disease.
Learn stress-reduction techniques
Living with a life-long condition like PsA can be stressful, and excessive stress can make symptoms worse and trigger flare-ups. To better manage mental health and PsA, aadopt some stress management tactics. When anxiety kicks in, try activities such as meditation, listening to music, going for a walk, talking to a friend, or practising yoga.It may take some time to get used to these activities, but they will help relieve stress to a great extent, which is an essential part of managing PsA.
Care for the skin
People with PsA may also have psoriasis. In such cases, keeping the skin moisturized especially after bathing or swimming may be a wonderful way to pamper the skin. It is recommended to use minimal soap to wash the body and wear loose-fitting cotton clothes to prevent skin irritation and discomfort. Psoriasis medications must be taken as prescribed.
Make self-care a priority
Spending just 15 minutes a day focusing on self-care and seeing to personal needs will likely improve the mood and overall quality of life.
Manage related health conditions
While PsA often coincides with psoriasis, some may be dealing with other health conditions at the same time. PsA is also commonly linked to obesity, heart diseases, depression and other mental health disorders like anxiety.
Depression, in particular, can significantly affect the management and treatment of PsA. As depression may interfere with seeking medical help (for PsA) or adhering to the treatment, it may complicate disease management. Gaining control of any other health conditions, especially mental health can help prevent PsA flare-ups and slow disease progression.
BEING PHYSICALLY ACTIVE
PsA causes joint pain which results in limited movement. Although specific exercises can worsen symptoms, others can help in several ways.
PsA causes joint pain which results in limited movement. Although specific exercises can worsen symptoms, others can help in several ways.
Here are some suggested exercises:
Tai Chi
It focuses on breathing, gentle movements, and meditation. This helps improve quality of life and depression associated with various forms of arthritis
Walking
It is a low impact aerobic activity that can help build strength and improve joint movements
Yoga
It improves strength & flexibility and it is known that people regularly practicing yoga have double pain tolerance than those who do not
Swimming
It can improve joint stiffness and relax the muscles
Light weight lifting
Lifting weights can help improve muscle strength and support strong joints. 2–3 days per week of weight training is recommended
Exercises that can worsen psoriatic arthritis
Be mindful about the exercises that may put stress on the joints and lead to additional pain or stiffness in a PsA patient. Here are some exercises to avoid:
Running
High intensity interval training
Playing outdoor games
Before and after exercising
PsA can adversely affect the hands and feet, causing stiff joints, pain and swelling. Several steps can be taken at home to relieve pain while exercising. Taking good care of the hands and feet can help prevent extra discomfort. Following the tips below before or after exercising can help:
Massage the wrists and arches of the feet
Wear gloves to prevent nail damage
Take breaks when exercising and walking
Use cold or hot compresses to relieve swelling or pain
Massage any stiff joints
Regular stretching of the feet and legs is a must
Inserts can help relieve pain from walking
Use proper footwear that provides support, stability, and has enough space to accommodate swelling
Exercising while having a flare-up
While there are many advantages to being physically active, it is imperative to avoid added restlessness or injury.Pacing is important. When experiencing a flare-up, choose to do short bursts of exercise like three 10-minute sessions instead of a 30-minute session.
Maintaining a good exercise routine
It is helpful to follow a consistent exercise regime to achieve good health. Here are some tips for maintaining a successful exercise routine:
WORK AND PSORIATIC ARTHRITIS
Why managing psoriatic arthritis at work is critical?
Apart from pain and swelling in the joints, PsA can reduce the ability to move freely and easily. Living with PsA can make a person feel exhausted. In order to maintain good health and well-being, and be productive at work, it is important for a PsA patient to find effective strategies.
How to thrive at work?
These tips can help improve the work experience of a person with PsA.
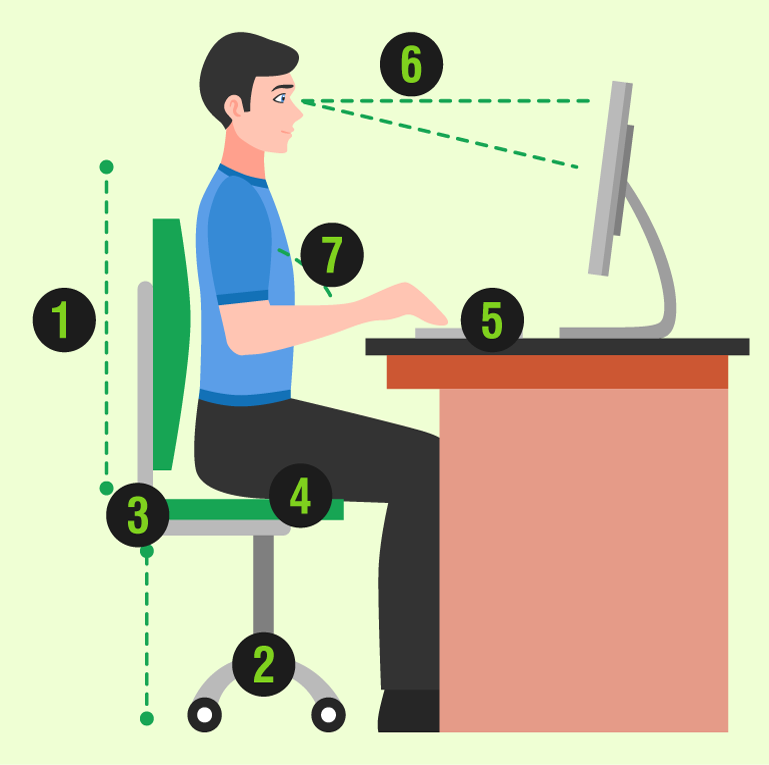
Setting Up a Comfortable Workplace
- Use a chair that has armrests and able to provide sufficient support to the lower back
- A wheelchair can help with mobility
- Do not choose a chair that has a seat which is too deep
- Seating position must be such that the feet are flat on the ground with a gap of at least one inch between the knees
- The mouse and keyboard should be at the same height
- Adjust the monitor height so that the top of the screen is at, or slightly below eye level
Good sleeping habits
People with psoriasis and PsA are more likely to have trouble sleeping, which may cause immense fatigue. Other consequences are as follows
Trouble concentrating
Weight gain and obesity, which may put extra stress on the joints
Difficulty remembering things
Mood changes
In addition, poor sleep can make joint pain worse, and may increase swelling. Recognizing the issues that are affecting sleep can help one find relief.
Symptom control is critical
Painful joints or itchy skin can make it difficult to get sound sleep.For those experiencing trouble sleeping or flare-ups, talk to a rheumatologist and dermatologist. They may adjust the medicines and suggest lifestyle changes that may help relieve the symptoms.
Experts say that light is a crucial timekeeper. Darkness and light help signal the body to sleep. Blue light emitted by devices such as phones and tablets cam disrupt a person’s body clock, which is why it is recommended that such devices are kept away before bedtime.
Diagnosing and treating sleep disorders
If the PsA symptoms are monitored properly and a person feels good but is still struggling with sleep, it is recommended that he or she sees a sleep specialist. But one should talk to a rheumatologist before doing so. Some sleep disorders that are commonly seen and require treatment in PsA patients include:
The healthiest solution is to identify the reason(s) for the sleeplessness and fix the problems that are responsible for causing wakefulness.
TRAVELING WITH PSORIATIC ARTHRITIS
Traveling can be very exciting, but it can also be stressful especially if a person has PsA. Besides thinking about where to stay,eat and what to pack, one needs to plan and think about managing PsA symptoms while travelling. The ideal way to stay away from vacation worries is to plan in advance. The right preparation can help avoid travel snags(like forgetting to take the medications on the flight), decrease the likelihood of PsA flare-ups,and stay pain-free during thestay.
Here are some tips to help manage PsA before and during the travel:
Check that the medicine prescriptions are current
Book a doctor’s appointment prior to the trip so the doctor can do a thorough assessment and offer tips for managing any flare-ups during the trip
Organize the medications and prepare two sets to put in two different bags for safe measure
Prepare to travel with items that provide comfort such as eye mask, ear plugs, travel pillow, hot or cold packs and a cane or walker
Given the likelihood of morning stiffness, plan outings for later part of the day
Use one’s own cosmetics including shampoo, conditioner, soap, moisturizer, sunblock and lip balm
Stock up the food bag with healthy snacks and plenty of water. Avoid eating junk food
In order to prevent stiff joints, move regularly and stretch throughout the flight
PREGNANCY AND PSORIATIC ARTHRITIS
One of the most significant decision couples make is whether or not to have babies. But for a woman with PsA, she has a number of factors to consider if she chooses to get pregnant. These include:
- What effect will arthritis or the medications have on the baby?
- Will pregnancy affect one’s arthritis or skin disease?
- Will the disease have any effect on childbirth?
- Will the new mother be able to care for her baby due to her physical condition?
Fortunately, in most cases, the answers are quite reassuring. For women with PsA, listed below are things to take note of right from the planning stage to delivery and beyond.
Is psoriatic arthritis hereditary?
Genetics does play a role in PsA. So, there might be a possibility that a child may develop PsA. However, it helps to know that many women with PsA go on to have healthy babies.
Effect of psoriatic arthritis and medications on baby:
Doctor may stop or change medications prescribed for PsA or skin disease. A rheumatologist should weigh in on some of the risks and benefits with regards to medications.
Disease activity during pregnancy:
PsA usually goes in an inactive state (with no flare-ups) during the nine months of pregnancy. But disease activity might vary after pregnancy.
Caring for new baby:
There is a possibility that a flare-up may occur after delivery and one might experience severe fatigue.
Here are some questions that a pregnant woman undergoing a PsA treatment can ask the doctor:
- Will PsA or its medications affect the baby's development?
- Will PsA symptoms deteriorate during pregnancy?
- Will arthritis affect one’s labour period?
- Will a new mother be physically able to care for her baby after birth?
- Can women take painkillers during pregnancy for PsA pain? If yes, which ones?
- Is it likely for a mother to pass PsA on to her child?
- Can a new mother breastfeed her baby while undergoing PsA treatment?




