WHAT SHOULD ONE KNOW ABOUT ULCERATIVE COLITIS?
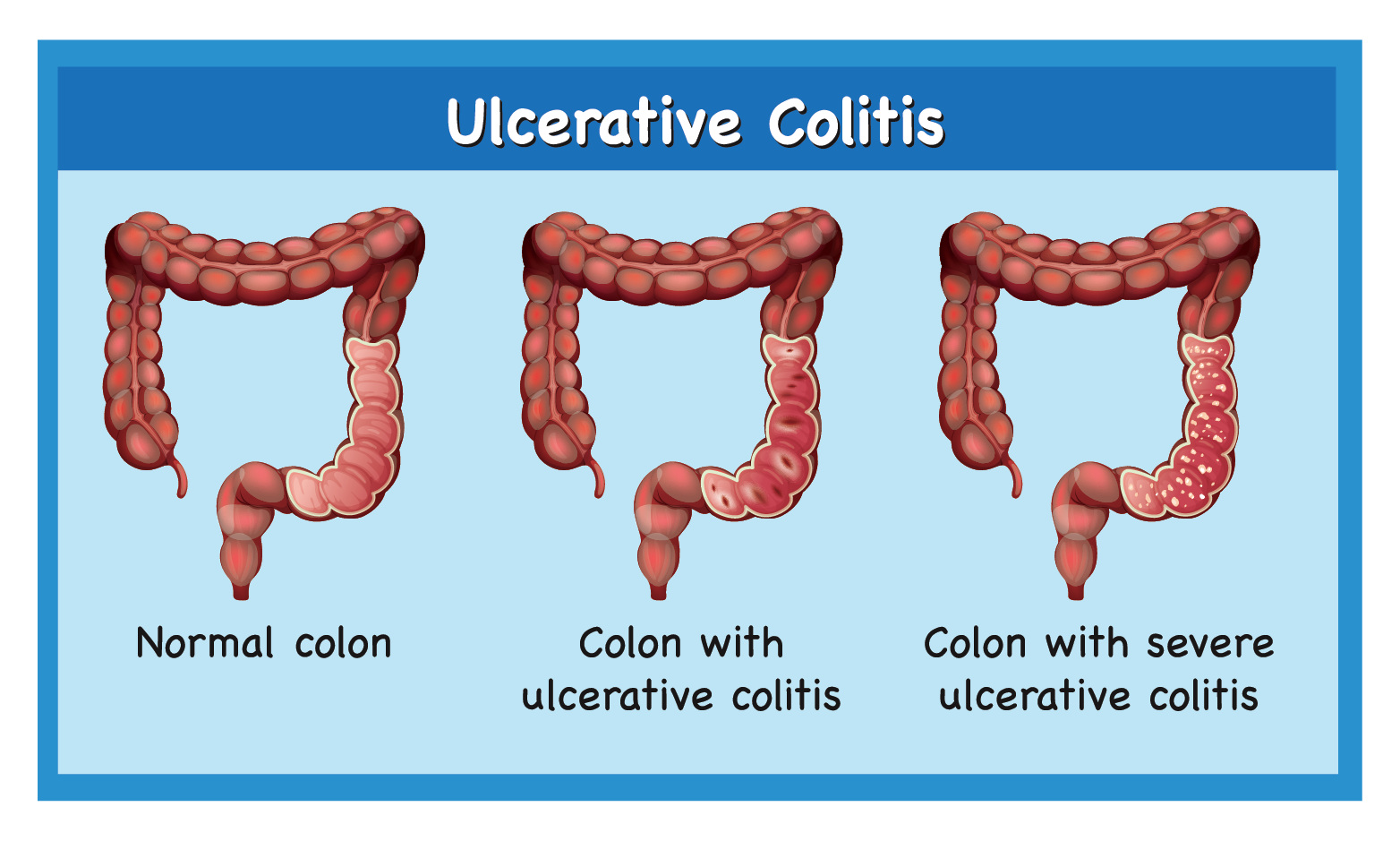
Ulcerative colitis (UC) is an ailment of the digestive system under a group of bowel diseases called inflammatory bowel diseases (IBD). This condition causes sores (ulcers) in the colon, which can lead to:

Abdominal pain

Diarrhea (watery stools)

Blood in the stools
It causes irritation, inflammation, and ulcers in the large intestine (also known as the colon).
Why does ulcerative colitis occur?
UC occurs when the immune system makes an error. Usually, it attacks invaders in the body, e.g. if one has common cold, the immune system will attack the germs that have caused the common cold. But in UC, the immune system thinks that food, good gut bacteria, and the cells present in the large bowel (colon) are the intruders. The cells of the immune system that usually have a protective role, attack the colon's lining instead, causing swelling and sores in the large intestine.
Who is at a higher risk of getting ulcerative colitis?
Numerous risk factors can make a person more vulnerable to UC. These include the factors one can control (i.e. diet and lifestyle) and factors one cannot control (i.e. age and heredity).
Following are some of the most common risk factors:

UC can develop at any age; however, it begins usually before 30 years of age

Increased consumption of polyunsaturated fatty acids and a sedentary lifestyle may contribute to development of UC

People with a family history are at higher risk

Certain bacteria or chemicals may trigger uncontrolled swelling in the colon
SPOT THE SYMPTOMS
What are the typical symptoms?
Symptoms of UC can differ based on the severity of swelling in the intestine and where it occurs. Signs and symptoms may include:

Diarrhea

Abdominal pain and cramping

Rectal pain

Passing small amount of blood with stool

Urgency to defecate

Inability to defecate despite urgency

Weight loss

Fatigue

Fever
LET'S UNDERSTAND FEW TERMS ASSOCIATED WITH ULCERATIVE COLITIS
Inflammatory bowel disease (IBD): The first important term to know is inflammatory bowel disease (IBD). This term is often confused with irritable bowel syndrome or IBS, an intestinal disorder leading to pain in the stomach, bloating, diarrhoea and constipation.
Inflammatory bowel disease is a group of lifelong illnesses. One type is UC, and the other being Crohn's disease. UC only affects the large intestine in most cases. But Crohn's can happen anywhere in the digestive tract, and can cause symptoms from the mouth to anus.
Remission: Remission in UC is a phase of no symptoms. One feels well in the remission phase, and UC doesnot interfere with daily activities.
Total Parenteral Nutrition (TPN): TPN is a method of feeding nutritional products to a person via infusion, It can be done in the hospital or at home.
Anaemia: A condition of having less than the normal number of red blood cells or amount of haemoglobin in the blood.
Bowel: Another name for the intestine. The small and large bowels mean small and large intestines respectively.
Colon: Large bowel or large intestine.
Colonoscopy: A diagnostic test which uses a thin, flexible tube with a lighted camera inside the tip and enables the doctor to view the complete colon and determine whether a person has colon diseases such as UC.
Constipation: A condition in which there is difficulty in emptying the bowels, usually associated with hardened faeces.
Flare -ups: The sudden surge of UC symptoms or the return of UC symptoms abruptly.
Gastroenterologist: A physician who focuses on diagnosing and treating illnesses of the digestive system affecting the food pipe, stomach, small and large bowels, rectum, liver, gallbladder, or pancreas.
Ileum: The lowest part of the small intestine that connects to the large intestine.
Pan-ulcerative colitis: A type of UC affecting the whole large intestine.
WHAT IF ULCERATIVE COLITIS IS NOT TREATED ON TIME?
UC is a progressive condition that does not improve on its own. If not treated, symptoms may continue to worsen, and swelling may spread within the colon (large intestine). There is also a risk of further injury to the lining of the colon with every flare-up. This can make it tougher for a person to cope with the condition going forward. Leaving UC untreated in children can limit and delay their growth and development.
If UC is untreated, it may cause:

Nutritional deficiencies

Loss of appetite

Swollen abdomen

Fatigue

Unintended weight loss

Anemia

Fever

Rapid heartbeat

Bleeding from the rectum

Ruptured bowel

Greater risk of colon cancer
Other complications may include:

Arthritis
Skin problems
Painful red eye

Bone loss

Liver problems
Remember, one does not necessarily have to face these complications if
a doctor's help is taken early on.
HOW IS ULCERATIVE COLITIS MANAGED?
When to visit a doctor?
One should immediately seek medical help in case of:
- Breathing difficulty
- Fast heartbeat
- High temperature (fever)
- Blood in the stools becoming more prominent
There is no specific trigger for flare-ups in most people, although a gut infection can seldom be the cause.
What should one know regarding the diagnosis of ulcerative colitis?
The doctor will enquire about one’s symptoms and their medical history first.
Subsequently, the doctor may carry out the following tests:

Physical examination
A doctor will check the abdomen or anal portion of a person for swelling, tenderness, or soreness

Blood / Stool Tests
To check for certain factors which are responsible for UC

Imaging tests
X-ray or CT scan to rule out serious complications and a detailed examination of the rectum and colon
Other tests that may be carried out include:
- Endoscopy: A doctor uses a flexible tube to examine one's stomach, esophagus, and small intestine
- Biopsy: A surgeon removes a tissue sample from one's colon for analysis
- Flexible sigmoidoscopy: A type of endoscopy, during which, a doctor inserts a long, flexible tube into the rectum so that they can examine it, the sigmoid colon, and part of the descending colon. Flexible sigmoidoscopy is also known as sigmoidoscopy
- Colonoscopy: During a colonoscopy, a doctor inserts a lighted scope called a colonoscope into the rectum to examine the inside of one's colon. It’s also a type of endoscopy
GOALS OF ULCERATIVE COLITIS TREATMENT
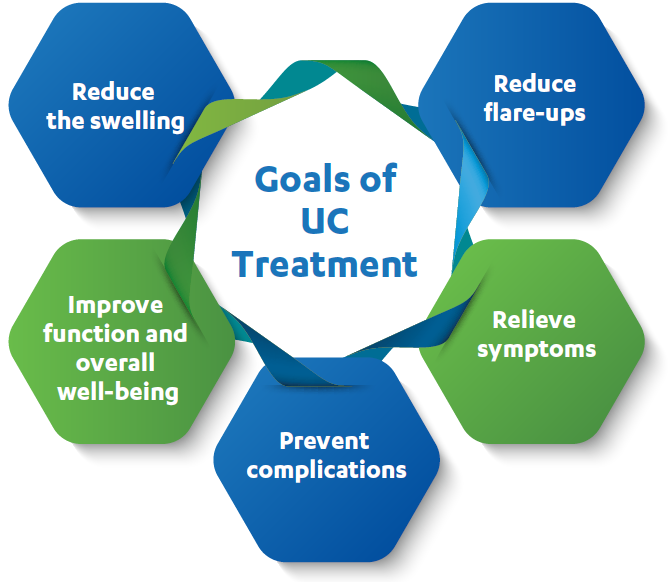
What does the treatment include?
Below are few treatment approaches for treating UC. The doctor will choose an approach that is best suited for an individual based on the condition and disease severity:

Lifestyle changes
Changes in the diet and certain exercises might help

Medications
Help in relieving pain, prevent or slow down the disease, and enable a person to live well

Surgery
Based on the disease severity, a doctor may recommend surgery which usually involves removing the affected parts of the large intestine (colon)




