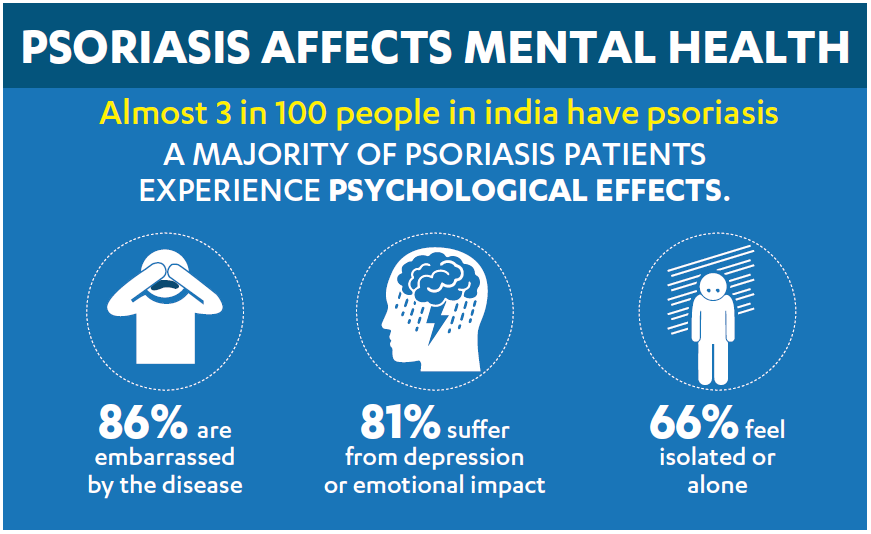
DOES PSORIASIS AFFECT MENTAL HEALTH?
Psoriasis is a lifelong condition and may have a negative impact on a person’s quality of life. According to a survey by the National Psoriasis Foundation, approximately 75% of patients believed that psoriasis had a moderate to severe negative impact on their quality of life (QoL), with changes in their daily activities.
Psoriasis affects how a person sees himself/herself and how others see him/her. Those affected often experience problems with their body image, self-esteem, self-concept, face difficulty in maladaptive coping responses.
How does psoriasis affect mental health?
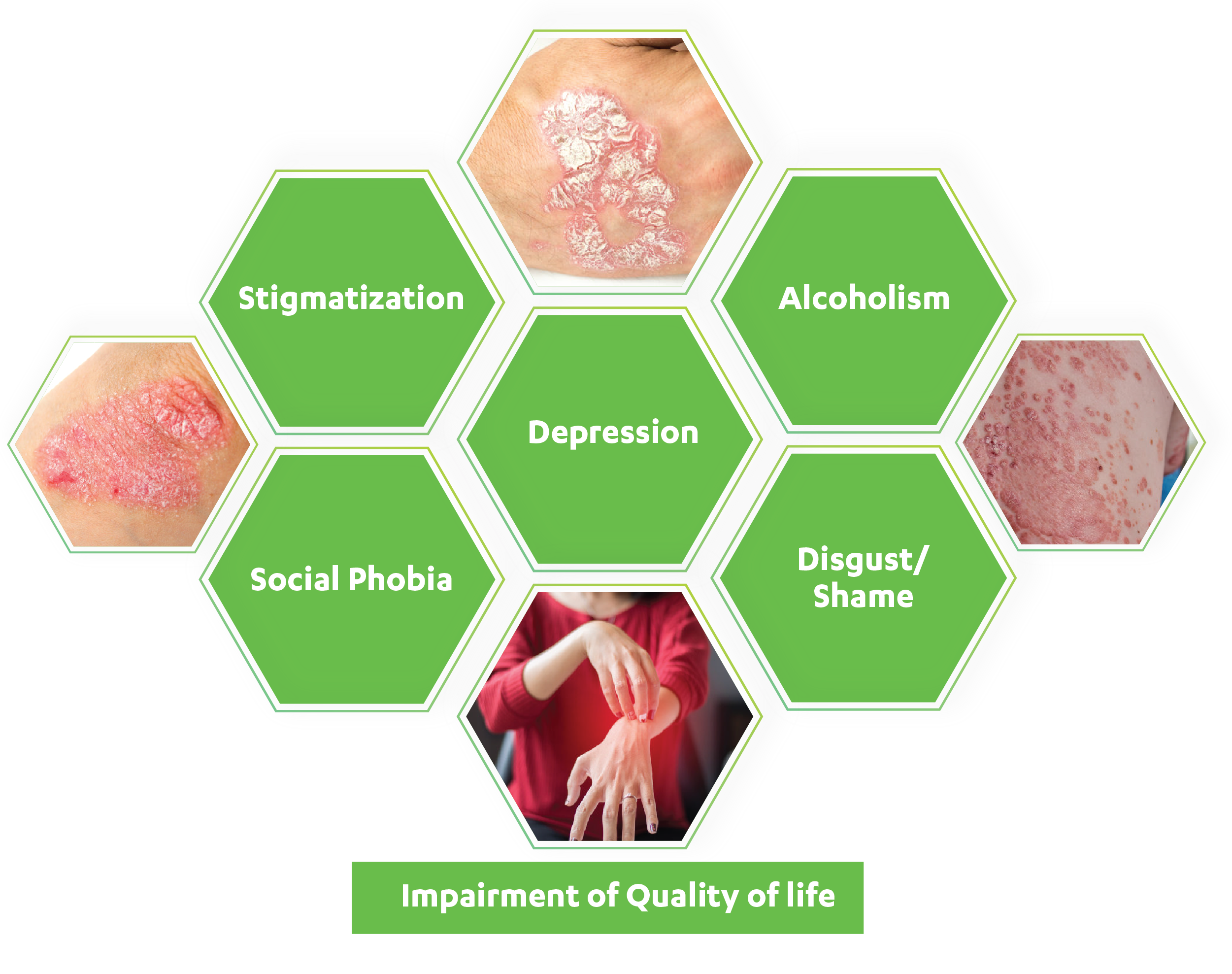
It has been estimated that the psychological impact of the skin disorder is severe in most patients with psoriasis. Psoriasis is associated with a variety of psychosocial aspects/symptoms. One might feel or have:
- Guilt, shame, embarrassment or helplessness
- Poor self-esteem and self-worth, occasionally causing social isolation
- Sexual dysfunction, due to self-consciousness or painful skin spots
- Suicidal tendencies that develop in severe untreated cases of psoriasis
- A person with psoriasis might have fewer professional opportunities due to discrimination or perceived restrictions on career choices, which can result in unemployment and financial difficulties
- Difficulties in doing daily activities, including dressing, bathing, and sleeping
- A negative impact on the patient's family relationship, including financial hardship, stress to the person caring for the psoriasis patient
- Stress, low or depressed mood can trigger flare-ups in psoriasis, causing poor quality of life
Psoriasis and mental health interrelation can be a vicious cycle
Experts say that psoriasis can worsen or contribute to several mental health conditions like depression, anxiety, bipolar disorder, eating disorders etc. The social stigma linked with psoriasis may eventually manifest as low self-esteem and poor psychosocial adjustment.Mental health problems like anxiety or depression may kick in or trigger and worsen psoriasis flare-ups. Vis a vis, studies have also shown that major stressful life events could also result in the new onset of psoriasis. Having psoriasis on the visible areas of skin can take a toll on one's mental health and can affect mood and interpersonal interactions in a negative way. These usually happen through self-perception and also through the reactions of others to the affected skin.
Treating psoriasis helps in maintaining a patient's mental health. Patients who continue treatment as per the advice of their dermatologist have better outcomes.
One must remember the physical attributes of psoriasis, the pain and fatigue that a patient endures are
challenging; but one has to be stronger than this disease.
MENTAL HEALTH AND WELLBEING CHECK-LIST
The K10 checklist is a simple measure of your psychological health. It uses a series of questions to rate certain aspects of your wellbeing, with results showing whether negative feelings, thoughts or emotions have affected your daily life.
This test should only take a few minutes to complete. It is important to be as truthful as you can. It is extremely common for anxiety and depression to co-exist with inflammatory disorders, but the good news is there are treatment and support options that can help.
Acknowledgement: “Professor Ronald C Kessler of the Department of Health Care Policy, Harvard Medical School is thanked for the use of research on the K10 funded by US Public Health Service Grants RO1 MH46376, R01 MH52861, RO1 MH49098, and K05 MH00507 and by the John D and Catherine T MacArthur Foundation Network on Successful Midlife Development (Gilbert Brim, Director).”
HOW TO COPE?
Most people think that psoriasis is a skin condition, but it affects many other body parts apart from one’s skin. Unlike a health problem like diabetes, psoriasis is visible to other people. It may be challenging to deal with. When a person takes care of oneself, they may be able to easily overcome emotional and mental well-being-related challenges.
It may help control psoriasis too.
Make stress relief a daily routine
- Be nice to self and do something nice every day to ease the effects of stress
- Make oneself a cup of herbal tea in the afternoon and enjoy that "me time" after waking up or before bedtime
- Seeking support from close people can help. With close people and family, one can have comfort and support, making it easy to deal with psoriasis
Treat the depression
One may feel extremely low and become sad with psoriasis, which may sooner or later cause depression.
Some symptoms of depression include:

Sadness

Guilt or worthlessness
Irritability and anger

No interest or pleasure in things they used to enjoy before
A person who is constantly in a low mood can also face the following symptoms:

Trouble sleeping

Fatigue

Mood swings

Trouble staying focused, making decisions, or remembering tasks

Weight loss or gain

Headaches or stomach aches

Social isolation
Depression, when treated with either medicines or therapy, can relieve stress.
Inform the doctor if the feeling of sadness remains for more than a couple of weeks. Reach out to a psychiatrist/psychologist to help deal with the condition.
Following additional tips may help a person deal better with the condition:

Consult a doctor: If there are symptoms of anxiety or depression, seek medical help. A doctor may prescribe medicines or recommend some lifestyle modifications.

Stay physically active: A steady exercise schedule can help one feel emotionally better. It can be a regular morning walk, gym training, or yoga session. Any form of exercise that one finds enjoyable may help ease the symptoms of anxiety and depression. Light activities may also help lower fatigue and pain.

Talk it out: When one is in pain, it is important to have someone to turn to. Most times, a simple pep-talk or a shoulder to lean on can be a good stress reliever.

Practice stress management techniques: Deep breathing exercises, meditation, progressive muscle relaxation may help one relieve stress and cope with the disease in a better way.

Join support groups: One may join support groups where people with the same condition come together and can listen to each other’s concerns related to their journey.

Consume a healthy diet: Excessive junk food intake may trigger swelling and cause pain and stiffness. A healthy diet containing fresh vegetables and fruits may help positively boost one’s physical and mental health.
Take control of the treatment
Many treatment options are available that can help relieve the symptoms and control disease progression.
It's entirely possible to reach a point where the skin is clear, and one can feel good about it. Usually, it is seen that the patients'moods improve, and they feel better about themselves and life in general, because they get relief from pain and irritation after taking the treatment. Please consult your doctor to understand the optimal treatment option for you.




